What Does Mips Stand For In Medicare

What is the purpose of mips and how does it work.
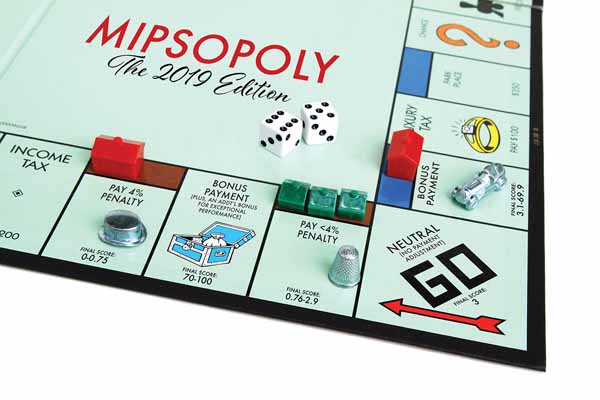
What does mips stand for in medicare. Discover more about how this will affect you here. Mips is the name of a new program that will determine medicare payment adjustments and is an acronym for the merit based incentive payment system. If you decide to take part in an advanced apm you may earn a medicare incentive payment for sufficiently participating in an innovative. Using a composite performance score eligible professionals eps may receive a payment bonus a payment penalty or no payment adjustment.
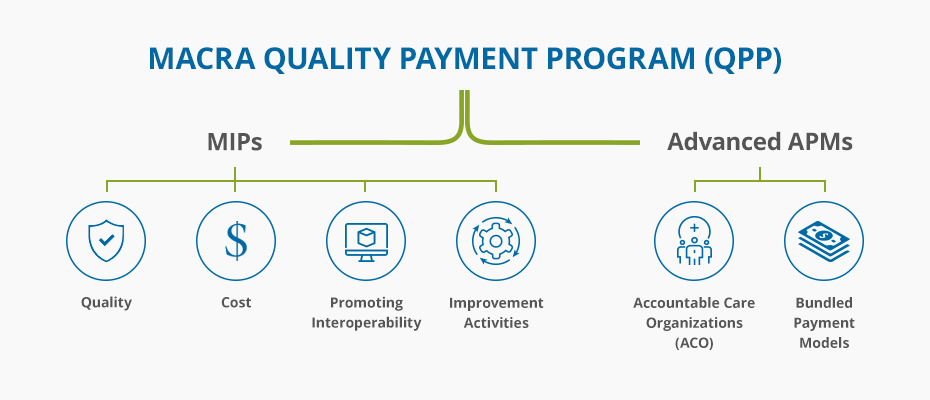
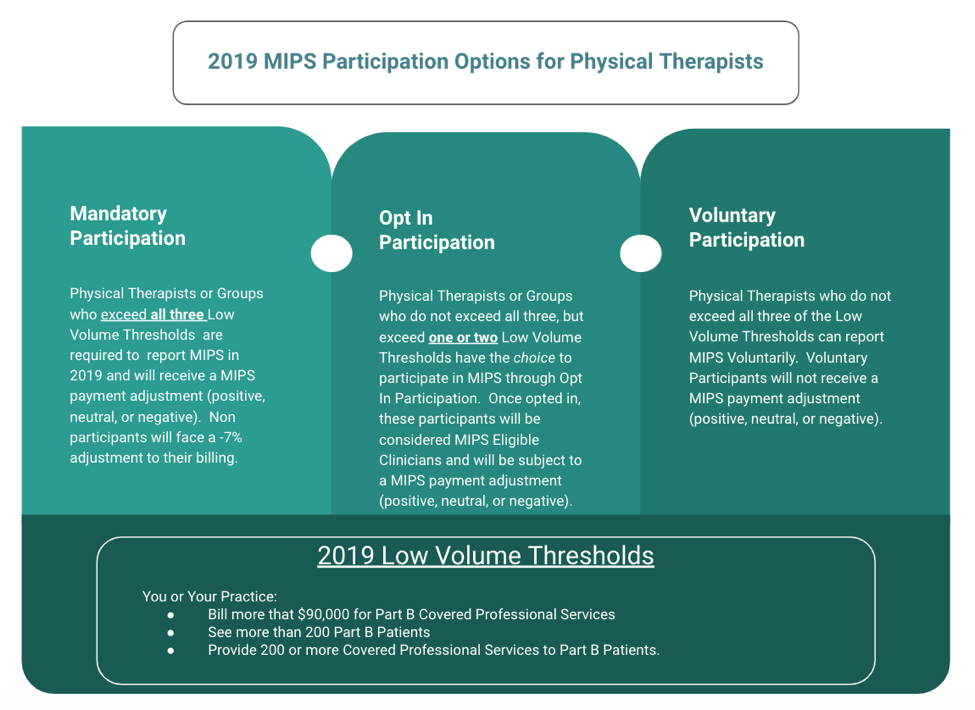
According to the department of health and human services hhs the centers for medicare and medicaid services. The medicare access and chip reauthorization act of 2015 macra is a federal legislation that required cms to create the metric driven merit based incentive payment system mips track of the quality payment program to reward clinicians for value over volume based on performance points scored according to national percentiles. What does mips stand for in healthcare. If you re a mips eligible clinician you ll be subject to a performance based payment adjustment through mips.
Mips scores determine medicare part b reimbursement and rate. A two track quality payment program qqp not in place emphasizes value based. Streamlines multiple quality programs under the new merit based incentive payments system mips gives bonus payments for participation in eligible alternative payment models apms macra also required us to remove social security numbers ssns from all medicare cards by april 2019. The medicare and chip reauthorization act macra is a law that changed how the federal goverment pays physicians.
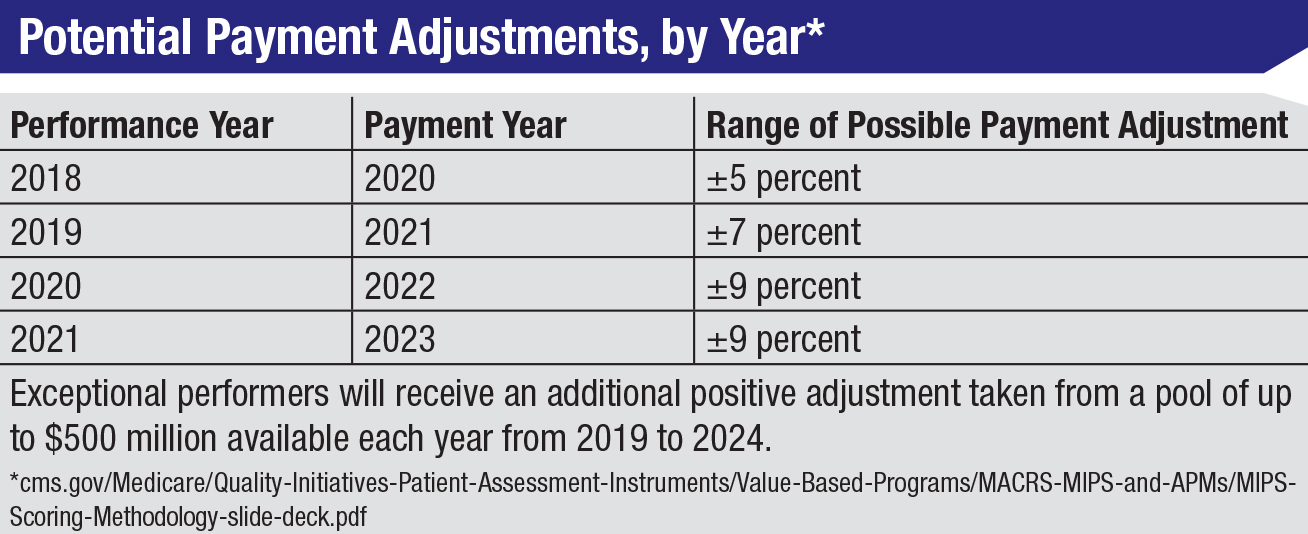
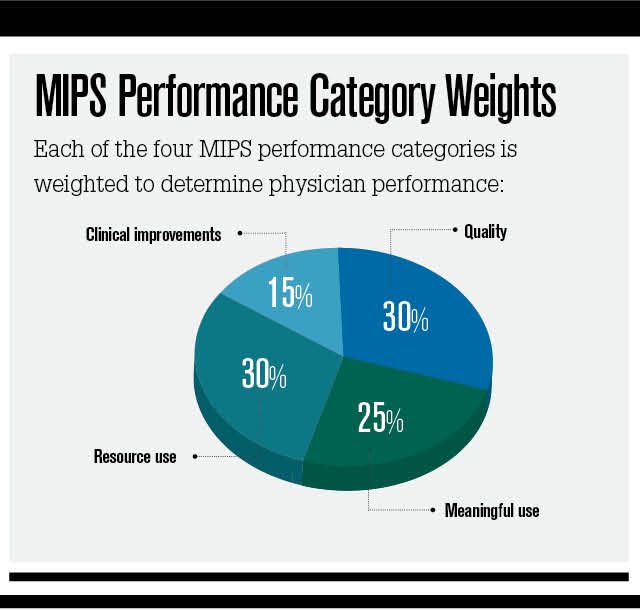
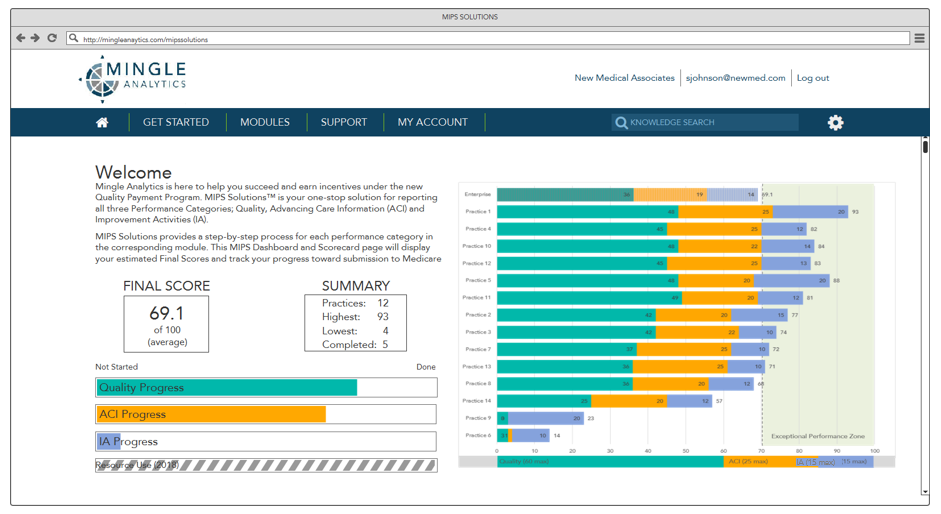
Advanced alternative payment models apms. The merit based incentive payment system mips. Mips payment adjustments reflect an eligible clinician s performance two years prior which means that payment adjustments for the 2017 transition year will be applied to medicare part b reimbursements starting on january 1 2019. Mips adjusts medicare part b payments based on performance in four performance categories.
Quality cost promoting interoperability and improvement activities. Mips will be performance based and the therapist s performance will be scored using performance benchmarks.